作者简介:蔡雷鸣,男,1980年生,技师,主要从事临床检验工作。
目的 探讨血清中性粒细胞明胶酶相关脂质运载蛋白(NGAL)检测在急性肾功能损伤(AKI)早期诊断中的意义。方法 收集无慢性肾病的重症监护病房(ICU)、冠心病监护病房(CCU)患者60例,分别在其术前及术后6、12、48 h采集血样,其中27例发生AKI(AKI组),以其余33例未发生AKI(无AKI组)。应用酶联免疫吸附试验(ELISA)检测血清NGAL浓度,碱性苦味酸法检测血清肌酐(SCr)浓度,胶乳增强免疫浊度法检测血清半胱氨酸蛋白酶抑制剂C(Cys C)浓度。以48 h内SCr高于基础水平50%作为AKI的诊断标准,应用受试者工作特征(ROC)曲线评估NGAL在AKI早期诊断中的效力。结果 与术前比较,AKI组术后6、12、48 h的血清NGAL明显升高,Cys C在术后12、48 h明显升高,而SCr在术后48 h才显著升高。无AKI组术前与术后6、12、48 h的NGAL、SCr、Cys C浓度差异无统计学意义( P>0.05)。术后6、12、48 h血清NGAL的ROC曲线下面积为0.51[95%可信区间( CI): 0.250.78]、0.80(95% CI: 0.580.95)、0.85(95% CI: 0.610.99)。结论 血清NGAL在术后6 h上升,术后12 h即能较好地预测AKI,其预测AKI时间早于Cys C和SCr。血清NGAL可能在AKI早期诊断中有良好的应用价值。
Objective To investigate the clinical significance of serum neutrophil gelatinase-associated lipocalin(NGAL) detection in early diagnosis of acute kidney injury(AKI).Methods A total of 60 inpatients in intensive care unit (ICU) and coronary care unit (CCU) without chronic kidney diseases were enrolled. Sera were collected before surgery and 6, 12 and 48 h after surgery respectively. There were 27 AKI patients and other 33 patients without AKI. The concentration of NGAL was determined by enzyme-linked immunosorbent assay (ELISA). Serum creatinine (SCr) was detected by Jaffé reaction method. Serum cystatin C (Cys C) was detected by Latex-enhanced immunoturbidimetry. AKI was defined as an increase in SCr of at least 50% from baseline within 48 h. The efficiency of NGAL in early diagnosis of AKI was evaluated by receiver operating characteristic (ROC) curve.Results Serum NGAL increased significantly 6, 12 and 48 h after surgery, while serum Cys C increased 12 and 48 h after surgery, and SCr increased 48 h after surgery in the AKI group. There was no obvious difference in the concentrations of NGAL, SCr and Cys C in the non-AKI group before and 6, 12 and 48 h after surgery ( P>0.05). By ROC curve analysis, serum NGAL 6 h after surgery had an area under the curve of 0.51 [95% confidence interval ( CI): 0.25-0.78], serum NGAL 12 h after surgery had an area under the curve of 0.80 (95% CI: 0.58-0.95), and serum NGAL 48 h after surgery had an area under the curve of 0.85 (95% CI: 0.61-0.99).Conclusions Serum NGAL increases 6 h after surgery and predicts AKI accurately 12 h after surgery. For predicting AKI, serum NGAL is earlier than Cys C and SCr, and shows that serum NGAL can be as potential marker for the early diagnosis of AKI.
急性肾功能损伤(acute kidney injure, AKI)是临床多发且病死率较高的疾病, 主要原因是缺乏早期、敏感、特异的诊断手段。临床现在用来判断AKI主要还是依靠血清肌酐(SCr)的检测[1]。但是肾脏有很强的代偿能力, 通常SCr的升高是出现在病程的中、晚期, 延误治疗时机[2]。最近的研究发现中性粒细胞明胶酶相关脂质运载蛋白(neutrophil gelatinase-associated lipocalin, NGAL)与AKI有极高的相关性[3], 可能对AKI早期诊断、预防、治疗和预后改善等方面有重要意义。我们主要探讨了血清NGAL在AKI早期诊断中的价值。
收集2009年1月至2010年12月上海市第一人民医院宝山分院无慢性肾病的重症监护病房(ICU)、冠心病监护病房(CCU)患者60例, ICU中的患者主要是外科大手术、多发性挤压伤患者, CCU的患者主要是造影剂介入手术者。AKI根据2007年制定的急性肾功能损伤小组(acute kidney injury network, AKIN)标准确诊, 60例患者有27例发生了AKI(AKI组), AKI发生率为45%, 其余33例列入无AKI组。分别在术前及术后6、12、48 h采集外周静脉血35 mL, 离心制备血清于-80 ℃冰冻备用。
NGAL检测采用酶联免疫吸附试验(ELISA), 试剂盒由丹麦bioporto公司提供, 仪器为BIO-TEK全自动酶标仪; SCr检测采用碱性苦味酸法, 试剂由美国Beckman-Coulter公司提供; 半胱氨酸蛋白酶抑制剂C (Cys C)检测采用胶乳增强免疫浊度法, 试剂由上海申索佑福生物有限公司提供; 仪器为Beckman Lx-20全自动生化仪。AKI诊断标准为48 h内SCr高于基础水平50%[1]。各项检测严格按照标准操作规程操作。
采用SPSS 16.0软件进行分析, 所有计量资料以
无AKI组术前与术后6、12、48 h的NGAL、SCr、Cys C浓度无明显变化(P> 0.05)。AKI组术后6、12、48 h的NGAL浓度均明显高于术前(P< 0.05)。AKI组术后12、48 h的Cys C浓度明显高于术前(P< 0.05), 而术后6 h与术前比较差异无统计学意义(P> 0.05)。AKI组术后48 h的SCr浓度明显高于术前(P< 0.05), 而术后6、12 h SCr浓度与术前相比差异无统计学意义(P> 0.05)。见表1。
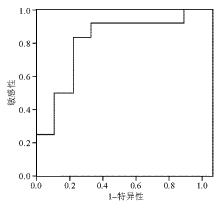
进一步用ROC曲线分析发现, 术后6、12和48 h血清NGAL的ROC曲线下面积分别为0.51[95%可信区间(CI):0.250.78]、0.80(95%CI:0.580.95)、0.85(95%CI:0.610.99), 见图1。当术后12 h的血清NGAL诊断值设为200 ng/mL时, 其诊断AKI的敏感性和特异性分别为91.7%、77.8%。
| 表1 各组NGAL、Cys C、SCr不同时间段的平均浓度 |
AKI是病死率的独立预测因子。在现阶段, SCr和尿量是国际公认的AKI诊断和分期标准[1]。但SCr并非一个敏感指标, 而且从SCr代谢与分布的生理学来看, SCr除反映肾小球滤过率(glomerulus filtration rate, GFR)外, 还受到其分布及排泌等综合作用的影响。目前比较一致的观点认为, SCr因易受年龄、体重、性别、种族、营养状态、蛋白摄入量等许多非肾脏因素的影响, 敏感性差。尿量更易受到血容量状态、药物等非肾脏因素影响[2]。因此, 一旦GFR下降、SCr上升, 肾功能损害往往已达到相当严重的程度。AKI诊断亟待更敏感的早期诊断指标。
NGAL是1993年在动物中性粒细胞中发现的与明胶酶结合的分泌型蛋白质, 相对分子质量为25 000, 属于脂质运载蛋白家族中成员[4]。在生理状态下, 中性粒细胞、肾小管上皮细胞、肺泡巨噬细胞、支气管上皮黏液细胞、胃壁细胞、小肠潘氏细胞、肝胆管细胞、胰腺细胞等分泌少量NGAL, 循环NGAL通过肾小球滤过, 在近端肾小管重吸收[5]。研究人员通过缺血性及肾毒性损伤动物模型发现, 在损伤发生后2 h内肾小管上皮细胞NGAL的转录表达有显著升高[6, 7, 8]。大量后续的临床研究也证实了动物实验的结果, 血液和尿液NGAL在不同年龄、不同疾病患者中都具有较好的AKI预测价值[9, 10, 11, 12, 13, 14]。
本项目研究对象为住院患者中AKI相对高发的ICU和CCU患者, 这些患者接受外科手术或放射造影剂的暴露有比较高的AKI发生概率, 并剔除了术前SCr异常的病例。因为慢性肾病患者的NGAL平均水平比较高[15], 本研究AKI的发生率为45%(27/60), 这与文献[14]报道的基本一致。本研究选择了术前及术后6、12、48 h共4个时间节点观察血清NGAL的变化规律, 发现血清NGAL在术后6 h开始升高, 术后12 h的血清NGAL能较准确地预测AKI的发生, 诊断值为200 ng/mL时, 诊断AKI的敏感性和特异性分别为91.7%和77.8%, 比目前公认的AKI标志物SCr和新的标志物Cys C的升高和预测时间更早。
由于受条件限制, 本研究没有检测尿液NGAL的变化规律, 多项研究表明尿液NGAL也能较好地预测AKI的发生。联合检测血和尿液NGAL的变化规律可能更好地预测AKI的发生。有文献报道, 正常人血NGAL浓度为5090 ng/mL[14], 尿NGAL浓度很低(< 5 ng/mL)[9], 本研究中无AKI组的血NGAL浓度为120130 ng/mL, 比文献报道的正常人高, 这可能是住院患者受到药物、疾病等多项干扰因素影响导致。
有研究表明血清NGAL的浓度高低能反映肾功能的受损程度[14, 16, 17], 本研究由于病例数不多, 没有做NGAL浓度与肾功能变化的相关性分析, 如果能进一步延长观察时间和收集更多病例, 对患者整个住院期间的肾功能进行跟踪, 将对进一步阐明NGAL在AKI中的临床意义有重要作用。
总之, 血清NGAL在术后6 h上升, 术后12 h即能较好地预测AKI, 其预测AKI时间早于SCr和血清Cys C, 这表明血清NGAL可能在AKI早期诊断中有良好的应用价值。
The authors have declared that no competing interests exist.
| [1] |
|
| [2] |
|
| [3] |
|
| [4] |
|
| [5] |
|
| [6] |
|
| [7] |
|
| [8] |
|
| [9] |
|
| [10] |
|
| [11] |
|
| [12] |
|
| [13] |
|
| [14] |
|
| [15] |
|
| [16] |
|
| [17] |
|